Every year many companion pets die from tick paralysis. Until recently the risk of tick paralysis was confined to pets that visited the coast or contacted a tick brought back from the coast, for example in rugs or vegetation.
However, we are now seeing tick paralysis in pets whose owners have not recently travelled outside of the Canberra region.
Paralysis ticks appear to have developed the ability to survive the cooler, drier Canberra climate and whilst more prevalent from August to March and after heavy rain, ticks are a risk to pets all year round.
Paralysis ticks are capable of killing a pet within three to four days of attaching, so don’t delay.
Early signs include tiredness, staggering, vomiting, breathing difficulty, progressing to paralysis. The signs may continue to worsen even after the tick is removed.
Although most pets treated for tick paralysis survive, prevention is much safer and far less expensive. Tick prevention products vary between dogs and cats. They also vary in efficacy as well as length of protection. Please talk with our staff about the most suitable tick protection for your pet.
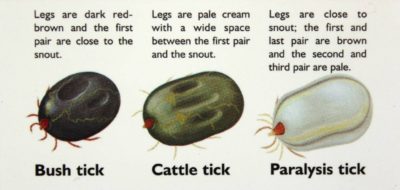
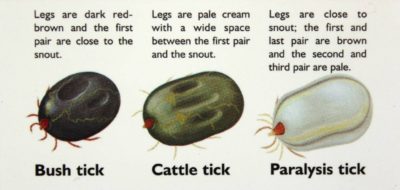
Not all ticks are dangerous. Bush ticks are occasionally seen locally but do not cause illness. The most effective action is, if you find a tick on your pet, bring it with you to the vet to be identified.
PREVENTION
TICK PREVENTATIVES
Newer products in the form of chewable tablets, such as NexGard and Bravecto are providing effective tick protection for dogs. The rinses and top spots that we previously used for dogs are less effective and can be toxic to cats that groom or have close physical contact with recently treated dog.
For cats, prevention options are more limited and we recommend Frontline® spray, although the Frontline® Plus top spot or Seresto flea collars may provide some protection.
DAILY SEARCHING
This is recommended even in pets receiving tick prevention treatment as none are 100% reliable. The ticks may attach anywhere but are more often found on the front half of the body.
CLIPPING THE COAT
Trimming the hair assists in searching for ticks. Be prepared, if your pet has a long coat and presents to us with suspected tick toxicity, we may want to shave their entire coat to aid the tick search.
If symptoms of tick toxicity are noticed, a thorough search of the animal should be made and a veterinarian contacted immediately. Do not offer food or water to animals suffering from paralysis as their inability to swallow may cause an aspiration pneumonia.
Ticks can be very hard to find, so don’t rule out tick paralysis if you cannot find one. There may also be more than one tick on the pet. If a tick is found on a pet which is not exhibiting signs, remove the tick by firmly grasping the tick close to the skin and plucking it off. Keep searching and remove any other ticks.
So long as signs do not develop, there is the option to keep your pet quiet and cool for 24 hours. Please keep the tick in case it is required for identification.
If you are at all uncertain, call for an appointment and bring your pet in for a vet check. Depending on the case, we may recommend home monitoring, or monitoring for signs in hospital
+/- treatment with anti-serum.
TREATMENT
Veterinary treatment of tick paralysis includes:
- Thorough searching and removal of all ticks. This may require clipping the coat.
- Application of a tickicidal wash or spray.
- Administration of tick anti-serum.
- Oxygen supplementation if necessary which may require transfer to an emergency centre for overnight monitoring or ventilation.
- Maintaining hydration using intravenous fluid treatment, until the pet is able to swallow and therefore eat and drink again.
- Keeping the pet cool, relaxed and comfortable
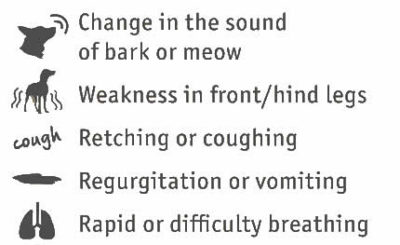
WHAT ARE THE SIGNS OF TICK PARALYSIS?
Signs of tick paralysis vary depending on the length of time the tick has been on the animal, as well as the potency of the toxin, which can vary between ticks.
Signs include:
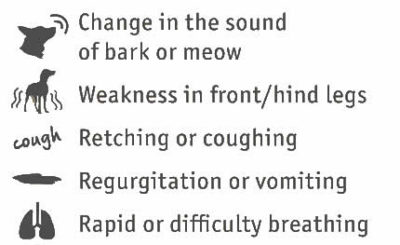
- A change in vocalisation
- Increased or laboured breathing
- Coughing
- Excessive salivation
- Vomiting or regurgitation
- Weakness in the hind legs, which typically progresses to involve the forelimbs
IF YOU FIND A TICK ON YOUR PET CONTACT YOUR VET IMMEDIATELY
The toxin produced by paralysis ticks is very potent. Even when the tick is removed, most animals get worse before they get better. This is because the toxin already in the animal’s body continues to circulate and attaches to nerves for a period of time. Remove food and water as your pet’s ability to swallow may be compromised, putting your pet at risk of inhaling food and developing aspiration pneumonia.





 Like people, many pets suffer from forms of anxiety. If your pet cannot settle during thunderstorms or fireworks or perhaps your pet cannot settle if you are not present, then talk with Dr Helen Purdam about some strategies to help the both of you cope.
Like people, many pets suffer from forms of anxiety. If your pet cannot settle during thunderstorms or fireworks or perhaps your pet cannot settle if you are not present, then talk with Dr Helen Purdam about some strategies to help the both of you cope.