Safety tips for Christmas time!
As we head into the festive season and look forward to relaxing with family and friends, it’s a good time to give some thought to keeping our pets safe as they join us in the fun festivities!

Here are some potential dangers to watch out for:
Some human foods are just not meant for dogs:
Chocolate, plum pudding, Christmas cake, fruit platters and delicious roasts and stuffing. What could possibly be wrong with sharing that!
Unfortunately, these Christmas goodies can contain ingredients that are toxic to dogs, including chocolate, sultanas, grapes, raisins, onions, garlic and macadamia nuts.
Signs will depend on the food that has been eaten and can be delayed. For example kidney damage from grapes and raisins may not become apparent until weeks down the track. If your dog has eaten something they shouldn’t have, please speak to a veterinarian immediately.
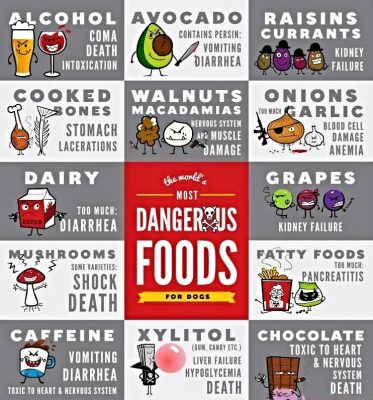
Alcohol
This is a no-brainer really but there is NO safe amount of alcohol for your dog to have. Effects will range from depression, difficulty walking, slow breathing, collapse and even possibly loss of life.
Overindulgence
Just a little bit of ham can’t hurt, right? Well, a little here and a little there adds up! We love to treat our pets but we need to remember that a little to us can be a lot to them, and eating too much of something different or high in fat is a very common cause of illness for them.
Overindulgence can trigger stomach pain, vomiting, diarrhoea and even pancreatitis (which can be fatal). Feeding cooked bones should always be avoided as these can cause bowel obstructions and constipation requiring intervention.
Don’t risk your dog getting treats from the BBQ or scavenging from finished plates. If you can’t ensure your guests will resist your dog’s pleading eyes, then you are better off to have your dog safely out of their way!
You need to take control here on behalf of your pooch, because they are not going say no!
Noise Anxiety
Parties, fireworks and summer storms make Christmas time hard for dogs who are prone to anxiety.
Nobody knows your pet better than you do. Always observe your mate closely and look for the subtle signs that they are worried, and take action.

Avoid the stressors where possible, and make sure they always have access to a quiet, safe retreat. Some pets will benefit from judicious medication to get through this time unscathed. Please call us if you would like to discuss.
The Christmas Tree!
Now, we’re not saying don’t have one! We like the festive fun as much as anyone, but here are a few things to consider if you do.
- Tummy upsets after chewing pine needles or drinking stagnant Christmas tree water.
- Electrocution is a risk if your pooch starts chewing the Christmas tree lights.
- Obstruction or injury to the bowel can occur if tinsel, other decorations, wrappings or ribbons are eaten.

So to make things easy, here’s a checklist on how to make your Christmas tree dog-friendly this year.
- Cover or box around the tree stand.
- Plastic cover the electric cord for the lights.
- Plastic or non-breakable decorations (no glass)
- Decorations secured in place.
- Tinsel up high out of reach (or none at all)
- Secure the tree so that it can’t easily fall.
Holiday Plants
Popular Christmas plants and flowers such as poinsettias, amaryllis, lilies, hibiscus, Christmas cactus, berries, mistletoe and holly leaves are all poisonous to your pets. Make sure they are out of their reach, as consumption could result in illness or even death.

Batteries & Toys
Swallowed batteries are very dangerous for dogs, causing a range of issues from burning their gut to a life-threatening obstruction or stomach rupture! Batteries are a common addition to Christmas gifts so please ensure they are kept well out of reach of your pooch.
Many toys contain small plastic, rubber or metal parts that, if eaten by a dog, can cause choking or dangerous gastrointestinal blockage requiring immediate surgery.
With a little careful planning, you can ensure your Christmas celebrations will be free of unnecessary trips to the vet. However, if you have concerns after hours during the festive season, please call:
Canberra Veterinary Emergency Services on: 62257257
Or
Animal Emergency Centre Canberra on: 62806344
We wish you and your furry family happy and safe holidays!
Reference to an article by Dr Claire Jenkins Co-founder of Vetchat.








 Behavioural problems in senior pets can result from medical issues like arthritic pain, loss of sight/hearing or diseases that affect the nervous system. They can also be attributed to age related deterioration of the brain known as Cognitive Dysfunction Syndrome.
Behavioural problems in senior pets can result from medical issues like arthritic pain, loss of sight/hearing or diseases that affect the nervous system. They can also be attributed to age related deterioration of the brain known as Cognitive Dysfunction Syndrome.


:max_bytes(150000):strip_icc()/itchy-dog-scratching-CharlesMann-E-getty-171154485-56a26b033df78cf77275656b.jpg)







