 Cats with diabetes mellitus have high blood glucose levels caused by a deficiency of insulin.
Cats with diabetes mellitus have high blood glucose levels caused by a deficiency of insulin.
Diabetes is commonest in older overweight cats. Male and Burmese cats are more susceptible.
Diabetic cats produce more urine and, to compensate for this, drink more.
Some cats saturate the litter rapidly or urinate outside the tray after being litter trained for years.
They also lose weight despite a ravenous appetite.
How is diabetes mellitus diagnosed?
If you report any of the above your vet will test for high blood glucose and glucose in the urine. Stress can cause a transient rise in glucose levels in cats so your cat may be admitted to hospital for a day for a series of blood glucose tests to confirm the diagnosis. Untreated diabetes eventually causes loss of appetite and lethargy.
How is diabetes mellitus treated?
Cats with diabetes are treated with twice daily insulin injections.
Diabetic cats require a low carbohydrate diet (unlike diabetic humans or dogs). Specially formulated diets such as Hills m/d are low in carbohydrate and high in protein and ideal for diabetic cats. Many small meals or grazing are fine as long as the cat is not overweight.
Some overweight cats get over diabetes if they lose weight. Stopping drugs such as prednisolone also helps.
What happens if my cat receives too much insulin?
We run regular blood glucose tests (known as blood glucose curves) to see if the insulin dose is correct.
Too much insulin drops the blood glucose dangerously low. Your cat might salivate, shake, walk unsteadily, convulse or faint. This is a hypo and is an emergency.
Rub liquid glucose, sugar solution, honey or icing sugar on the gums of an unconscious cat or syringe it into the mouth of a cat that can swallow. Call your vet as soon as you have done this.
Prevent hypos by double checking the dose of insulin every time you draw it up and by taking your cat for regular blood glucose curves. Cats often go into remission and don’t need insulin any more. The first sign of remission could be a hypo if we don’t check blood glucose levels often enough.
If your cat is off food or vomiting for more than a day do not give the normal dose of insulin. Call your vet.
You should never change the dose of insulin without first discussing it with your veterinary surgeon.
For more information visit


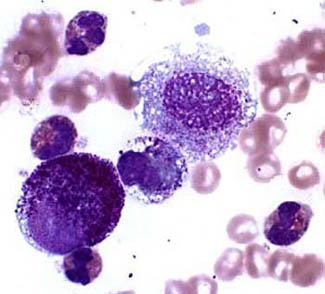 Mast Cell Tumours are aggressive skin cancers and common in dogs. They can look like anything: a patch of dry skin, a raised red itchy area, a wart or a lump.
Mast Cell Tumours are aggressive skin cancers and common in dogs. They can look like anything: a patch of dry skin, a raised red itchy area, a wart or a lump.